Wellness When You're Chronically Ill Isn't What You Think It Is
When you hear the word "wellness" these days, what comes to mind? Probably green smoothies, expensive supplements, or someone telling you to optimize your health at all costs. That version of wellness is NOT what we're talking about here.
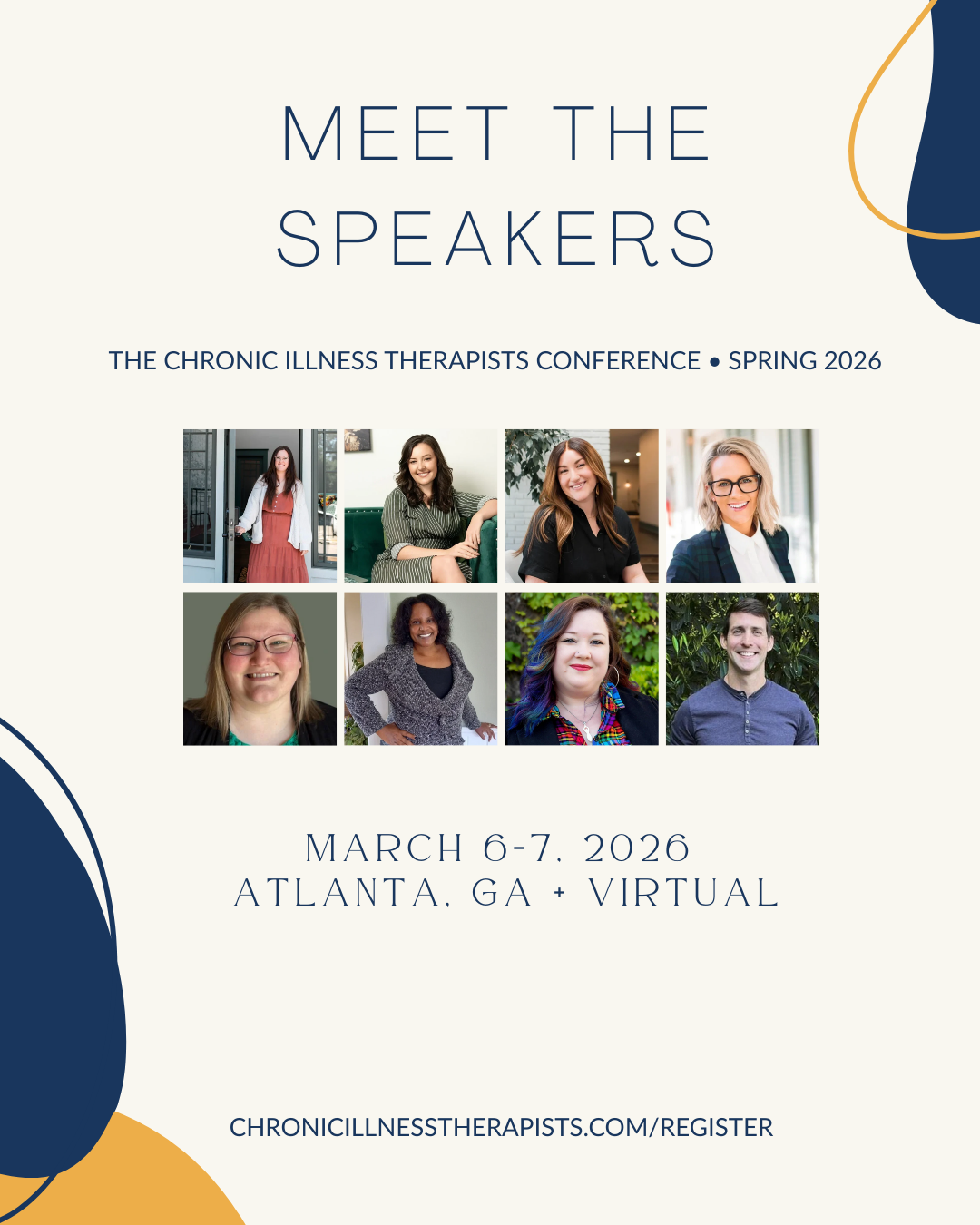
I sat down with Dr. Victoria Rodriguez, a Licensed Professional Counselor to talk about what wellness actually means when you're navigating chronic illness. Victoria specializes in medical trauma and is my amazing co-facilitating the Chronic Illness Therapist Conference with me this March 6 & 7th, 2026. This conversation was full of real talk about accommodations, systemic barriers, and why your comfort actually matters.
Wellness Is Seasonal (And That's Okay)
You know that wellness wheel we all learned about in grad school? The one with eight different areas like financial wellness, career wellness, social wellness? Victoria pointed out something that should be obvious but often isn't: you can't focus on all of those at the same time when you're chronically ill.
Instead, wellness is seasonal. There are seasons where you can focus on one type of wellness, and seasons where another type takes a backseat. And that's not failure. That's just reality when you're living in a body that has limits.
This shifts the whole conversation. It's not about balance across all areas all the time. It's about recognizing what season you're in and working with that.
It's Easier to Change Your Environment Than Your Body
Victoria introduced us to the social model of disability during our conversation, and it reframes how we think about ourselves when we consider our health. The medical model says people are disabled because something is broken with their bodies or brains. But the social model says it's actually about the environment.
She gave a perfect example from her own life. When she was working in community mental health, constantly on her feet and running from client to client, she had to take one sick day a week. But when she started working from home, where she could get up later, have all her medications nearby, and control her environment, she didn't need those sick days anymore.
Her body didn't change. Her environment did.
This is huge for therapists working with chronically ill clients. Instead of asking "how can we get your body to do this thing," we can ask "what accommodations can we build into your environment so your body doesn't have to work so hard?"
This is exactly why Dr. Victoria and I are co-facilitating the Chronic Illness Therapist Conference this March 6 - 7, 2026 in Atlanta—we're not just talking about these accommodations theoretically, we're building them directly into the experience.
Secure your spot now for 13 specialized CE hours you won't find anywhere else.
Your Comfort Actually Matters
Victoria said something that stuck with me: "I always talk about, especially for wellness, that your comfort really does matter."
When you're uncomfortable or feeling unsafe in a space, your brain is so focused on finding comfort that it's hard to remember anything else. You can't access your higher-level thinking. You can't problem-solve. You're just trying to survive.
So whether you're a therapist creating your home office or working with clients, prioritizing comfort isn't indulgent. It's necessary.
Some ways to do this:
Invest in a chair that actually supports your body
Control the lighting in your space (lamps, adjust screen settings)
Build breaks into your schedule between clients
Give yourself permission to work fewer hours if that's what your body needs
Let clients know they can sit on the floor, bring you to their bed virtually, move around during session
And if you're working in an agency where you don't have much control, we suggest starting yourself off with a needs assessment. Notice throughout your day: when am I experiencing tension? After my third client? In the morning? And when I’m feeling most at ease?
This helps you identify where accommodations would make the biggest difference.
The Messages We've Inherited About Rest
Something Victoria said really hit me: "I think in the US in particular, we really dislike being comfortable."
She continues on to explain: Think about it. Cashiers standing for entire shifts. Teachers needing accommodations just to sit while teaching. We've built a culture that sees comfort as laziness.
And a lot of us are the first generation in our families who can even have conversations about wellness. Victoria shared that she's the first person in her family who can take a nap in the middle of the day. Her parents and grandparents didn't have that option.
So when you feel guilty for resting or for needing accommodations, remember: you might be the first one in your line who's had this choice. That doesn't mean you don't deserve it. It means your parents deserved it too, and didn't get the chance.
Accommodations Are About Wheelchairs, Aid, and So Much More
When we think about accommodations, we often picture the obvious ones: wheelchair ramps, talk-to-text readers. But for those of us with dynamic and invisible disabilities, accommodations look different.
Maybe it's having a fragrance-free environment because some days you're really sensitive to smell. Maybe it's texting instead of calling because you're dealing with sensory overload. Maybe it's asking to step outside of a loud coffee shop mid-conversation because you're getting dysregulated.
Victoria emphasized checking out askjan.org, which lets you search by diagnosis or even just by symptom to find possible workplace accommodations. You don't have to know exactly what you need yet. Just start exploring what's possible.
Self-Disclosure as a Therapist: When and Why
We also talked about boundaries around self-disclosure when you're a chronically ill therapist working with chronically ill clients. This is something I get asked about constantly.
Here's my approach: I do disclose, but I'm very intentional about it. I mention it on my website, and in session I'll bring it up when I notice a client is over-explaining their symptoms because they're scared I won't understand.
When I say "I actually live with chronic fatigue and migraine too," and they stop over-explaining and can finally get to the point they actually wanted to make, that tells me the disclosure was helpful.
But Victoria gave an important caution: don't center your medical experience in a way that colors their decisions. Clients will ask what treatment you did, what worked for you. And that's where you have to be careful, because your experience isn't theirs.
The purpose of disclosure isn't to make it about you. It's to create safety so they can explore their own experience more deeply.
Building Wellness Takes Community
One thing Victoria kept coming back to: community can actually change your perception of pain. Community can help with pain management.
This isn't just about having people who understand your condition (though that matters). It's also about having people who can help with practical stuff: childcare, elder care, even just someone to complain to without judgment.
Sometimes the first step in any kind of wellness work is just being able to name the problem. To complain, as Victoria put it (using it as a neutral term). And having a community that validates that? That's powerful.
What We're Building at the Conference
All of this conversation is why Victoria and I are so excited about the Chronic Illness Therapist Conference we're hosting in March. We're not just talking about these accommodations theoretically—we're building them in.
Fragrance-free environment. Sensory room with low lighting and places to stretch out. Flexible seating (the room is double the size we need so people can sit on the floor, use blankets and pillows). Air purifiers throughout. KN95 masks in welcome bags. Fifteen-minute breaks between each talk. Virtual option for people who need to attend from home or bed.
We even created an Executive Functioning Package where we handle your hotel, some transportation, and give you an Atlanta City Pass so you don't have to think about logistics.
Because here's the thing: you deserve to show up to a professional conference and feel comfortable. You deserve to learn without your body being a barrier. You deserve rest built into the day, not just tacked on at the end when you've already pushed past your limit.
Wellness when you're chronically ill isn't about doing more. It's about creating environments that support your actual body and brain, not the body and brain you wish you had.
This blog post is based on an interview with Dr. Victoria Rodriguez on The Chronic Illness Therapist Podcast. For more resources on navigating healthcare challenges, subscribe to our newsletter and follow us on social media.
If you're a therapist who wants to learn more from Dr. Victoria Rodriguez, join us in the Chronic Illness Therapist Conference this March 6 - 7, 2026 in Atlanta (GA + Virtual). Click button below to secure your spot now.
Disclaimer: Everything we discuss here is just meant to be general education and information. It's not intended as personal mental health or medical advice. If you have any questions related to your unique circumstances, please contact a licensed therapist or medical professional in your state of residence.
Listen to my full conversation with Victoria Rodriguez on Ep 117: Wellness When You're Chronically Ill Isn't What You Think It Is
-
Episode transcribed with AI and may contain errors that are not representative of the actual word or meaning of the sentence.
Destiny Davis LPC CRC: [00:00:00] If you're a licensed medical professional and you're listening to this podcast, I already know that you're amazing at what you do.
but treating chronic pain and illness is work that's complex. It's messy. It hits finances. It hits health anxiety due to diagnostic uncertainty and. Prognosis
and also the most intimate parts of your client's lives like sexuality, generic CE courses. Simply don't prepare you for that, and that's exactly why we built the Chronic Illness Therapist Conference. This is not another general mental health course. It's 13 approved CE hours for both therapists and physical therapists in the exact nuanced topics that you all have been asking for for a while, like integrating financial therapy, navigating diagnostic limbo, deep clinical work on body partnership, like helping clients be less scared of their body while navigating scary conditions.
This conference is really an invitation to stop relying on generalized tools. if you're a physical therapist, a licensed professional counselor, a certified [00:01:00] rehabilitation counselor, a social worker, this is the specialized training that moves your practice forward.
Tickets are moving fast for both the in-person and virtual experience, so we'd love to encourage you to secure your spot and your 13 ces. Right now by clicking the link in the show notes.
The struggles you're having in the therapy room are not unique to you, but they often feel like we are all alone in them because no one's really talking about it. This is an evidence-based, nuanced, highly specialized set of speakers who bring both lived experience and professional experience.
In what we think is the most impressive way. We would love to see you there. We are hoping that our first year is such a success that we can continue doing it year after year, and we really do need your help to make that happen.
Go secure your spot and your 13 CES right now because the link is in the show notes. The episode will be waiting for you as soon as you're done. By the way, you can use the Code EARLYBIRD for $100 off a professional or executive functioning package ticket.
The Chronic Illness [00:02:00] Therapist Podcast is meant to be a place where people with chronic illnesses can come to feel, heard, seen, and safe. While listening to mental health therapists and other medical professionals talk about the realities of treating difficult conditions, this might be a new concept for you, one in which you never have to worry about someone inferring that it's all in your head.
We dive deep into the human side of treating complex medical conditions and help you find professionals that leave you feeling hopeful for the future. I hope you love what you learned here, and please consider leaving a review or sharing this podcast with someone you love. This podcast is meant for educational purposes only.
For specific questions related to your unique circumstances, please contact a licensed medical professional in your state of residence.
Destiny Davis LPC CRC: [00:03:00] Dr. Victoria Rodriguez is a licensed professional counselor in New Orleans, Louisiana. She's a recipient of the 2024 Louisiana Counseling Association Distinguished Professional Service Award, and was named the 2023 outstanding doctoral student by the Gamma Chapter of the International Counseling Honor Society.
In her private practice, she specializes in medical trauma and provides trainings on Wellness for professionals and healthcare organizations. Additionally, she serves on the Pregnancy Associated Mortality Review Board with the Louisiana Department of Health to improve equitable medical care in Louisiana.
And Victoria is going to be one of our speakers, and she's also my co-facilitator of the Chronic Illness Therapist Conference in March, 2026. So, so excited. Victoria, thanks for doing this podcast today.
Can you tell us first a little bit about your work and what drew you to focus on wellness in the context of chronic illness and disability?
victoria: like a lot of other therapists who provide chronic illness, uh, [00:04:00] focused therapy. I have multiple chronic illnesses myself, and something that I would hear not so much in the chronic illness community, but outside of it is that. should not be focused on wellness or health, um, because we are already sick, right?
So how can you focus on wellness when you are already dealing with so many doctor's appointments, um, dealing with flare-ups, dealing on days where you just don't have that many extra spoons or executive functioning? And so I think sometimes there can be this message to chronically ill people that there isn't time or space to focus on wellness.
And for yourself, you might have to change what wellness looks like for you or how it's defined when you're in a body that is just, um, unwell, right? So wellness can be subjective for each
Destiny Davis LPC CRC: Yeah, I think it's important to say and define because wellness right now has a very loaded connotation. I think, um, people on this podcast have heard me talk a lot about this, but yeah, it is [00:05:00] kind of like optimize your wellness and like there's this kind of push for being the healthiest body you can possibly be, and it's like at all costs.
And that's not what we're talking about here. We're talking here about how to simply live a life that you wanna live no matter what kind of health and, and health problems that you have going on in your body.
with that?
victoria: abs, know, when I think of even the wellness wheel, you know what I'm talking about, where it's like the, what is it, eight area, eight areas of wellness that we're up to, you know, for Yeah. a
financial wellness, career
which I'm really
excited about. cause we'll be talking about all of
at the chronic illness conference.
Like we'll be breaking them down by, by speaker, by topic. Um, but I think about that wheel and I think about, you know, when you're chronically ill, can you focus on all of those at the same time? What does balance look like in all of those eight areas of wellness? I tend to think of wellness now. Uh, and the literature would support this says [00:06:00] seasonally, like there are seasons where we can focus on one type of wellness and maybe seasons where another type of wellness takes a backseat,
Destiny Davis LPC CRC: exactly. And yeah, maybe we can talk a little bit more about. Um, that was kind of the, the goal of the conference is to bring all these different wellness aspects, financial, wellness, sex and, and relational wellness, um, family and like, you know, that kind of relational wellness as well as, uh, just like your relationship with your body.
Those are all different topics that we'll be having at the conference. And in your talk specifically is gonna kind of go into maybe some of the more systemic and indu and institutional barriers that your client, that our clients face when trying to, access like healthcare and wellness in general.
So maybe we can talk a little bit about that. Maybe some, some of the common systemic barriers that our clients tend to face.
victoria: talk a little about, about theory, right? Who is not excited to talk about theory, um, underpinnings of this [00:07:00] talk. So, you know, when we think about wellness and how about wellness is defined. I like to go back to the social model of disability. So there's like the medical model of disability that says people are disabled or unwell because of their bodies, right?
Or their brains. However, when we look at the social model of disability, the social model of disability says, actually, it's more to do with the environment. So I'll give an example for myself. Uh, for those of you who have worked in maybe community-based settings or nonprofit settings, when I was working in that setting and just on my feet a lot, or having to run from client's home to client's home, I was having to take like, I think at one point, like one sick day a week, right? But when I started working for myself from home where I could. Get up later in the day where I could have access to all of my care items, all of my medications in the home. was amazing how I no [00:08:00] longer had it to take, and I no longer had to take all of that time off. when we talk about wellness, whether it's for our clients or for ourselves, I like to focus on the idea that it is so much easier to change a environment to support your wellness than it is to change your brain or your body.
And sometimes it's impossible to change your brain and your body. So this talk is gonna focus and I, I hope this conference kind of. Relates to that, where when you're in this space, um, even at our hotel in Atlanta, that you can find items and spaces to support your wellness rather than having to force your body to find some kind of wellness or to force your body, um, to sit up or be uncomfortable or, or feel, um, any sort of flare up.
We're hoping that the environment itself can be built to support your wellness so that you can show up fully as yourself and, and ready to
Destiny Davis LPC CRC: Yeah, this is like, um, I learned this a lot in my somatic [00:09:00] experiencing training, but one thing that they kind of bake into their training is. Letting clients know that in session, like, you can sit on the floor, you can bring me to your bed, you can bring me to the couch, like virtually. If we're, I'm assuming we all are doing virtual.
Um, of course this in, in office though, in your own office, if you're doing, if you're seeing people in person, um, invite them to sit on the floor, have comfy blankets and pillows, and make it inviting in that way. Um, or like different kind of chairs. People can sit in different positions and also have the permission to like get up and move or eat or drink during session.
All of those are ways in which, um, even within our one hour sessions, we build in accommodations so that people are not feeling like they're, sometimes I, you know, my clients and I love them so much when they do this, they, they come with a list of things that they wanna talk about. Right? And I love it.
Uh, we do tend to get a lot done in those sessions, but I always want them to know like, Hey, this is not lecture hour. It's not about you coming here to like learn and do this thing really well. I want you to be comfortable, you know. [00:10:00] Things like that. So maybe you can speak a little bit more. I was just speaking to the client side and how, how clinicians can invite clients to be more comfortable.
Maybe you can speak a little more to like the therapists themselves being more comfortable in their own space.
victoria: couple of weeks. I'm not sure if this episode will be out by then, but you can catch the replay of, uh, the home-based practice. So living well for therapists who have telehealth practices, uh, while managing your own chronic health issues. And so first and foremost, I think just having control over your environment or as much control as possible is a big factor in your comfort. I always talk about, especially for wellness, that your comfort really does matter. We know that from the literature, when you are feeling uncomfortable or unsafe in a working space, it's so much harder to remember, um, any of your theory, you know, the hierarchy of needs. It's hard for you to remember all of those things when your brain is so focused on finding comfort. so I think it can be a really [00:11:00] radical act even in your home office. To prioritize comfort, whether that's finding or investing in a really comfortable seat that meets your body's physical needs, especially if you're chronically ill or have any sort of, um, joint issue or, or bone issue. Um, just giving yourself permission to invest in those, um, higher end supports in your home office.
Um, additionally lighting in your office, so maybe investing in lighting that's more appropriate for your eyes. Investing in a quality laptop, um, where you can change the lighting settings, uh, noise as well. So having control over the noise in your environment. Just a lot of sensory things in your home environment. additionally, and you can, might be able to speak to this as well in, in your telehealth practice, but I, I think about also just your schedule. So maybe your brain, um, or body can't handle more than like five sessions in a row. [00:12:00] Maybe accommodating yourself by adding breaks into your schedule. Or maybe exploring if you can even see five clients a day or 20 clients a week, you know, if that's appropriate for your body. I think these are some really hard conversations that we're gonna be having in this talk and at this conference, and I, I just couldn't be more excited to have conversations with therapists that are ready to prioritize their comfort and
Destiny Davis LPC CRC: Yes. It took me a long time to add breaks in in between clients. It was like, yeah, but if I take like extra, an extra 15 minutes or 30 minutes in between clients, then I'm like finishing my day later. And that was when I still had this mentality of like, just push through, get to the end, and then you can rest.
And I think what we're talking about is building rest. Whether that's sensory rest or physical rest or emotional rest into your day is how you get through.
victoria: think in the West in particular, well I'll say in the US in particular, we really dislike being comfortable. Like we are actively against comfort. [00:13:00] give an example. Go to your nearest grocery store and you'll see cashiers, uh, standing the whole time. That's just not how it's done in other countries or teachers.
So, for example, my partner is a teacher and when he had an injury, had to seek an accommodation to even just. Be able to sit and teach at the same time. we have all of these messages that are built in, uh, quite literally, that you should be able to stand for eight or 12 hours at a time or move eight or 12 hours at a time when that's not accessible.
Uh, not only to chronically ill bodies. Um, I, I, I think a lot of bodies, it's, it's pretty difficult to not have access to seating, uh, for long extended periods of time.
Destiny Davis LPC CRC: Yeah. What would you say to a clinician who is currently working, so if we're speaking to therapists, they're actually like sitting all day, but maybe a physical therapist is like more so standing all day. What would you say to them? For those who are working in an agency where they don't have a [00:14:00] lot of autonomy over that, like
where do you start with with them?
victoria: So first
I would do a needs
and we're gonna be doing that at the conference as well in my talk. Um, is first and foremost you wanna assess where those needs. One tool that I love to use for this is I identify it as a tension list. So you can just write on your phone throughout the day. When am I experiencing tension? Is it in the morning? Is it when I see after my third client? After my fifth patient for that day? So first and foremost, we wanna identify those points where there are tension, either psychologically or physically for your body. then we can start looking at physical accommodations for yourself. I will say the example that you gave for PTs, average PTs are really good at identifying accommodations for themselves. Um, so for example, I have a lot of PT friends that will even holding their bodies correctly or making sure that they're giving themselves breaks when working with [00:15:00] clients. Um, sorry, or patients. however, I would think if I did have a PT in front of me that was having issues setting up accommodations for themselves, I would also get really curious about what. Barriers are there, is it that you are in an agency setting and you're maybe not given that choice? Um, is it your own psychological barriers about what it means to ask for accommodation?
So I think it would be really important to differentiate between that. Um, and then another great website. Destiny. I know you love this one as well. Is the, is it, is it Jan, is it ask jan.com or Jan? I think it's just jan.com.
Destiny Davis LPC CRC: Yes,
no, it's askjan.org
org
victoria: Gotcha.
Destiny Davis LPC CRC: I only, I only know I've messed it up
times and so now I know it.
victoria: guys and they will have a list of by the diagnosis or by the disability. So let's say you're someone with a DHD, [00:16:00] can go in and search ADHD, and it'll give you all the possible accommodations. Now, that doesn't mean that you'll need every single one, but just all the possible protected accommodations that you can request at work. Um,
Destiny Davis LPC CRC: will even give you by symptom. So maybe you don't even have a diagnosis, but you know you like live with chronic pain or chronic fatigue. You can literally search chronic fatigue and click it and it will give you accommodations just for that symptom.
victoria: even to start your own brain working on what accommodations you want to request at work, um, because you deserve to feel comfortable at work and you deserve, um, and have a right to the accommodations that are afforded
Destiny Davis LPC CRC: Let's talk a little bit about what some of the other barriers are. Let's just kind of give a, paint a picture for what people are struggling with in their everyday work life, whether that's agency or at home. Um, let's just paint that picture.
victoria: they [00:17:00] struggle with with wellness. Um, so first of all, I think it's really important to take a macro look at this. Explore what are some systemic barriers that you're working against? So maybe your workplace doesn't have enough breaks built in. Um, maybe your schedule doesn't have enough breaks built in. And the reason I say systemic barriers is it's really important to maybe separate that self blame that can come up with wellness of, ugh, I'm not able to work out today, or I'm not able to quote, eat he or eat right today. And it might be because you quite literally don't have the brain space or the time to make that happen for you. Um, so I'd first look at systemic barriers and, and one way maybe to figure that out for yourself. A really simple exercise that I like to do with a number of my clients just taking out a piece of paper. Writing down things completely within my control, things kind of within my control, and then things completely outside of my control. maybe what we wanna focus in, in this talk in [00:18:00] particularly, is things within your control. And you might not even realize all of these things that are actually outside of your control, or you might be surprised by the things that are actually in your control. Um, so that's the first step I would take.
And when I think of barriers to, to wellness, I, I also think about the own messaging that we receive, especially as therapists, right? So this conference is for allied health professionals that specialize or, or want to learn more about chronic illness. And I maybe challenge that a number of us already know, um, we need to do for our own wellness. Right. And so I would be really curious about maybe the psychological or physical barriers that we're coming up against. Um, so again, maybe that looks like your current schedule that you're facing. Maybe it looks like systemic barriers, like being, um, a single parent or facing, um, [00:19:00] facing poverty, right?
Like the working poor, I think about when we were students, um, graduate students or working as LPCs, um, where we just did not have the income to prioritize our wellness. So I wanna be aware of that.
Destiny Davis LPC CRC: That was definitely like when I was working agency, I mean, and I felt like I couldn't take a break in between clients. It was because like, I need to get in and get out and then get home so I can relax. Like that was, you know, there was some mindset work. I definitely did and, and could have probably done more of, but that systemic barrier was huge.
And so that, just to kind of give some more context will be Megan Stevenson. She will also, she's also been on the podcast for this, she'll be doing a talk around finances and fi and, you know, management of, of finances, both from a, a mental, um. From a mindset perspective as well as logistics, and that absolutely plays into all of this.
You know, now that I, I don't work in agency anymore, I have so much more flexibility and had [00:20:00] to work through some of the mindset blocks to allow myself to take that flexibility so that I could
good for myself and my clients.
victoria: Yeah, um, what supports do you need to get around those barriers? So maybe it's like childcare or elder care, you know, are there supports that you need in that area? Do you need, um, someone to help, I know this, I don't have this, but maybe someone to help with laundry, like someone to help with, um, with household chores.
So, again, I know that's not accessible to everybody, but just getting a look at least of what you need first so we can have that conversation. Um, about like physical barriers as well of, um, just maybe the way that your house is, is set up your, your home or your business. I think, kind of like what we talked about earlier is it's set up to your sensory profile. Um, I'm wondering if there are other barriers that come up for you around this
Destiny Davis LPC CRC: Yeah, I think, um, The mindset stuff is important. [00:21:00] Um. The, the around, not just like the shoulds and you know, I should be able to do more, I should be able to push through this. But also, again, the money piece, like am I really, you know, am I gaining more or losing more by giving myself an extra 30 minute break in here and maybe I'm losing some money, but is that as long as I can pay my bills, like is that loss in finances actually going to long term, probably improve my finances because I'm giving myself breaks and keep in on, you know, it's more sustainable.
Um, so it's like, it's little things like that.
Um, yeah,
victoria: I love of us can practice wellness on vacation. Um, can we take that back maybe without all of those supports? Yeah. I
Destiny Davis LPC CRC: exactly.
victoria: too is sometimes when I'm
'cause really what we're talking about maybe too is the guilt or the shame that can come up with prioritizing your wellness. you know, when, when I'm having a flare up, something that I'm trying to remind myself is this [00:22:00] is the whole point. The whole point is for you to lie on the couch and do nothing. You set your business up like this. You set life up so that you could have this, this is something that you would've dreamed about working in community mental health, and it's time to take advantage of that now. so I think that's, that can just give us an example of how pervasive some of these messages are. Um. That we sometimes are our own greatest barriers in some instances.
Destiny Davis LPC CRC: Yeah, it's protective, right? We are trying to protect ourselves from the backlash we might receive from society or our agency or our family if we start to incorporate wellness. I mean, I think some of the messaging people receive, and this is just speaking to the barriers again, the messages is like, that's selfish.
That's, um, who do you think you are like doing all that? I wish I could have done that when I was your age. You know, I'm thinking about our parents maybe, or we get some of these really kind of toxic messages that say you should not be taking care of yourself because I wasn't able [00:23:00] to. Um, even if you have a chronic illness, even if you are living in chronic pain, like we all had to do it.
So you do too.
victoria: not the first, but like one of the first generations even that can have these conversations around wellness. So I know like my parents or grandparents' generation, um, the conversations around wellness looked very different and access to wellness looked very different. so I'm thinking like I'm kind of the first one in, I'm the first one in my line of family that can like, take a nap on the couch randomly in the middle of the day. You know, my, my. Family Yeah.
have access to that beforehand.
I think also sometimes for some families there can come that guilt of um, you know, my parents for whatever reason just did not have access to rest or prioritize rest in the same way. And when my mom experienced um, kind of similar symptoms like migraine, she would just push through it or do a load of dishes or do a load of laundry. Like there [00:24:00] was no, there was no rest. So I think when you feel yourself feeling well, I'm feeling like I should be doing this, or I'm feeling guilty for resting, um, I think it's really important to remember that you might be the first one, uh, in your family that's maybe even had the option of rest.
Destiny Davis LPC CRC: Yeah. Yeah. And then how do you grapple with that? You know, do you let that kind of guilt kind of eat at you like, well, I don't deserve this because nobody else in my family got the opportunity to, or do you start to turn that around and, you know, I, I see that privilege more as a, not an obligation that's too strong of a like word, but I see it as a, yeah, like my personal obligation to do what my parents deserved to do, but couldn't.
They deserved it too. Just 'cause I get to in, indulge in it doesn't mean that I deserve it. And they didn't. They simply didn't have that opportunity.
victoria: know, the whole point is that we're working less or, or hopefully, you know, able to [00:25:00] work less than ever before. And the, and the whole point is to, to access more rest, um, or more, more play time, more off time.
Destiny Davis LPC CRC: How do you help clients, or even how can therapists start to navigate their own tension between pursuing wellness and accepting their limitations?
Just like things are a lot harder from, for us, right? So like a lot of, like, I'm generalizing, but let's say we have chronic fatigue. It might be a lot harder for us to get through our laundry, right? So then we're kind of like fatigued by the end of it, and we have to do the laundry or we have to do like these certain things in our home have to get done.
So there's this tension I find with, um, with clients and with other colleagues as well around doing what's best for our body and actually like getting things done given the limitations that we tend to have with our physical symptoms.
Maybe we can just describe that tension a little bit more.
victoria: in, I'm like, yeah, I wish that you didn't have to. I wish we did not have to [00:26:00] ask these questions of I really need to go Yeah. I'm
in a lot of pain. Well, I don't
That you should have to go to work Yeah. a lot of
pain.
I don't think it's right that we make,
accommodations so difficult to, to access. Um, and I know that's not very Yeah.
oriented, but it's, it's so hard to
I, do have a lot of clients that come in, you know, sometimes I'll get clients, um, or therapists that will come in and say, you know, the problem is I rest and I still don't feel good, so what's the point in resting? Um, and I think that can be such a personal question based on disability. So you might have a dynamic disability, meaning that one day you can feel perfectly fine and then the next day you're crashing, or the next week you're crashing. And it's so difficult because one week you can do the laundry and then the next week that's just not accessible for you. Um, so I think it's really Yeah. So Go ahead. yeah, like we were just starting to have that conversation right there. Like, some days I can do this [00:27:00] and some days I can't. And how do I accept that for myself? Um, and it, you know, when, when we're talking in that realm of dynamic disability, usually for me, the conversation ends up looking like, then how do you one trust that your body is gonna come out of that flare up at some point, and you'll be able to get these things done again, but also without overdoing it now, like, you know, those days where you have your energy, so you kind of do all of the things and then you crash and burn.
Destiny Davis LPC CRC: So it's a lot of learning what your limits are when you feel good and when you feel not so good. Um,
yeah.
victoria: to figure out
your limits, figuring out where your limits are per day. And I, I think for some of my clients, it can almost be really frustrating when they can't figure out those limits right away. And so maybe setting up your expectations. And what I mean by that is can we have. Healthy expectations for what your body and brain can do on some days versus other days with the [00:28:00] recognition that at least for the time that you're in therapy with me, we're, we're just experimenting. We're experimenting with what accommodations work for you. You know? And when I think about laundry issue, for example, which, you know, we have ai, I really wish we would've had self doing laundry before we had that.
Um, but we don't. And so when I think about if laundry is really difficult for your body, what physical accommodations can we put in place? Like legitimately, can you buy clothes that you can wear more often, um, that you're not having to wash as often? Which by the way, was something that was around for hundreds and, and thousands of years before where we are today, where we're having to like Yeah, like just do loads and loads of more laundry. Right. Um, can you have like a step stool to your la I, I, for me, it's really hard to like grab clothing and then bend over. So can you have like a physical system set up in your laundry room that works for your body? So that's the first question I start asking with clients [00:29:00] around physical limits is what are accommodations that we can change in your environment to support your body, whether you're low energy or high energy for that week, or low pain or high pain for that week.
Destiny Davis LPC CRC: Absolutely. Yeah. And for, you know, clinicians, when your therapists, I mean, when your clients come in and, and they're saying, my goal with you in therapy is to learn how to get all my laundry done again, and, you know, not let this illness, uh, take over my life. What we're talking about here is, is the actual reframe and it's the actual goals that we end up putting in treatment plans.
The, the, the treatment plan goals. Goals become, can my client name three accommodations that help them? Blah, blah, blah, blah, blah. When they are in a flare up, rather than can we help them stop catastrophizing so that they can get their laundry done, like that's not.
victoria: like. Well, you can also get an [00:30:00] occupational therapist on your team. They specialize. This is what they do is they help you
Destiny Davis LPC CRC: Yeah.
victoria: what you wanna do in your life and
there. Um, among other, like allied health professionals, I think as therapists we can also focus on the emotional barriers that are either, either, yeah, like you said, the, the emotions that can come up when your body is not performing in the way that you wanted it or expected it to. Um, and also maybe there barriers to you accessing those accommodations, um, psychologically or systemically? Um, so I definitely would suggest even having conversations with your clients or yourself around, I need an occupational therapist or a physical therapist on my team so that I can figure out accommodations for these
Destiny Davis LPC CRC: Yeah, exactly. Sometimes it's leaning into doing less or not being, uh. Is perfect with some of these tasks and sometimes there are really good accommodations that can actually help you get the task done without depleting all of your [00:31:00] energy. And absolutely occupational therapy is like gold for that.
This weekend, this, this podcast will come out after, but the replay will be available for people. And I am interviewing, or I am having a, um, my workshop guest is an occupational therapist who's going over all kinds of strategies for, um, dealing with sensory overload, especially during the holidays. 'cause that's a big one.
And that's just something, you know, and again, something we don't think about when we start to talk about accommodations. We, we tend to think about like a talk to text reader for someone who, who's blind or a wheelchair ramped for someone in a wheelchair, but. For those of us with dynamic disabilities and, and especially invisible ones, a lot of us tend to have that sensory overload in one way or another.
And I don't know about you Victoria, but for me, like some days I am really sensitive to light and sound and other days I can handle it just fine. Um, and so it's, it's learning how to accommodate yourself in the moment and also not feeling like you have to always accommodate yourself [00:32:00] for the same thing in the exact way, otherwise people won't believe you.
'cause that's another thing that, that I know people really have a, um, a hard time working through feeling like they're not believed for good reason. 'cause a lot of society does not believe them. And so this is some of the identity stuff that you'll be talking about as well in, in your talk.
Yeah.
victoria: What I'll be talking
just self-care for wellness, but community care. know from the literature that community can actually change our perception of pain.
Community can help as pain management. I would ask if you have a community that you can go to you feel like you're having a high pain day that you can process these things with. Do you have a community that you can rely on to maybe help with some of these tasks that we talked about? And I know that that can be such, I, I feel absolutely so [00:33:00] lucky and so privileged to have such a supportive community, but it is so necessary to access, um, any type of wellness if you're managing chronic
Destiny Davis LPC CRC: Yeah. Can you describe what some of the things are that your community give you that you might be helping people and, and clinicians can help their clients to look for these things when they're building their community? Like what are some of the benefits that you see from, from the supportive community that you have?
victoria: not just for myself, but other people that can include, um. care, it can include childcare or elder care. Um, so maybe on high pain days, having someone at that level, it can include, um, even just emotional support. So even if it's just a virtual chronic illness group that you're able to join once a week or once a month, just being in that group and being able to complain, and I use complain as a neutral term, I think sometimes it can have this negative connotation. Um, the first [00:34:00] step is always complaining, right? Like identifying what the problem is. Identifying maybe these quote unquote negative emotions that you're having, and just having them validated in a group can be so powerful. I'll get a lot of therapists that will come in and say, well, I don't know what to say if my client is grieving this chronic health issue. And I'll say, well, you know, what we know from the research is that even just or virtually being there with that client is a, factor. In their wellness is a huge factor in how understood they're feeling, how held they're feeling through that grief. Um, so I would say that's, that's a big part of, of my community support.
Destiny Davis LPC CRC: Yeah. Yeah. When you're feel, when you're feeling heard and understood, it reduces this tension in your own body. So your clients, when you're working with them again. Yeah, I hear that often too. Like they feel like they want, they need to do more like therapists. They, they need to do more. And it's like you might be the only person in their life who validates that the way [00:35:00] that they're feeling is totally normal and okay, given their situation.
Um, and that doesn't mean it's okay in the sense that they should just stay there forever. There might be things that they can do to help better their situation and there might not be depending on. Um, and so hearing them and listening to them reduces tension in their brain and in their body, which actually gives them the capacity to start to problem solve for themselves, which is ultimately what we want.
We want our clients to have their own solutions to their problems because those solutions are typically gonna be the ones that work best for the client.
victoria: them listen to their own body and, and listen to their own need.
I, you know, when I think about as it relates to wellness, I think about cultural context, right? Whether that's disability, culture, um, ethno cultures, um, and, and all the subcultures that, that come along with that, right? Like there's, um, intersecting identities, [00:36:00] I think about maybe messages that you've heard in your family or in the larger society in your culture about wellness and what it means to be well. so for example, maybe you were part of a family um, was a pick yourself up by your bootstraps kind of family. Like you just kind of work through the pain. Um. I am in a family. So uh, I'm in a family that I was raised in, uh, south Florida, so, uh, Miami, a lot of, um, Cuban Americans. And in my family, you, you push through the work, but you make sure everybody knows it.
So you make sure that people, like that was your way of communicating, Hey, I'm in pain. Um, is just maybe telling family members, Ugh, I'm in so much pain, but I have to do the dishes. No, no. Let me finish this chore. Um, so there, could be a lot of ways that maybe your [00:37:00] family also talks about pain and identity and that maybe helps to in your development of your own identity and how you relate to wellness or, or chronic pain. yeah. I'm curious if that's something that you see with your clients as well.
Destiny Davis LPC CRC: Yeah, absolutely. This is a question that comes up quite a lot, um, from other health professionals like. What do you do as a therapist with working with chronic illness or, or, you know, again, they might think that coming to therapy means dealing with the anxiety. 'cause the anxiety is what's causing their pain.
'cause that narrative is out there a lot. And, um, we're actually, if, if I'm bringing up childhood dynamics and trauma and stress from childhood, it's not in the, I'm sorry to say it's not in the Gabor mate, your trauma caused your illness. Um, I I do think Gabor Mate has some great kind of theories, uh, out there and also some problematic ones.
So I'll just leave that there. But, um, [00:38:00] it's, it's not that your trauma caused your illness, yes, we do know a lot about how stress impacts the body and that can turn on certain genes for autoimmune conditions. I'm not dismissing that part of the science, but what I work on more so with clients is how their family dynamics show up and how they're taking care of their illness.
So it's like. Do you push through because that's what your family did, or do you chastise yourself for like, not being strong enough because you feel weak because of, of your illness? And, and that usually comes from dynamic family dynamics that had nothing to do with the condition. You know, maybe it's just how your family talked about, you know, your grades were never good enough, or you, everything you did was never good enough.
Especially in more abusive situations, um, physical harm and, and highly, highly emotionally abusive situations. You are going to mimic those, those dynamics to yourself. Um, and so when you need something, you're gonna respond to yourself the way that your family [00:39:00] responded to your needs. Again, whether that was in an illness way, um, related to an illness or not.
So that's what I work on.
victoria: it could get when we have families, um, or larger society that will straight up say, you're not sick or you can't be sick. Um, I think a lot of clients who have even invisible illnesses will find this to be accurate. And so when you're trying to work on your wellness, it, it might be, or, or an area of wellness, it might be really frustrating because you've received all of these messages that you're not sick. But then you actively are, you are actively experiencing chronic pain that is a barrier to you accessing wellness or working, um, on one of your areas of wellness. And so that can just be so and cause a lot of self gaslighting and self-questioning about your own identity a disabled person or your own relationship to illness.
Destiny Davis LPC CRC: Yeah, exactly. And that's why [00:40:00] we become this kind of pillar of validation because the validation in and of itself, a lot of time. Our clients, clients just did not get that, like, nearly as much as they needed to. So that, that's the purpose we serve for a lot of it.
Are there any unique boundary considerations that we, as therapists, especially those of us with chronic illness, need to think about when it comes to working with clients with chronic illness? Um, yeah. Just thinking about like self-disclosure or how much we are, you know, talking about medical versus like the, just the therapeutic role.
Like what are just some boundaries that we, we maybe need to start to think about when it comes to working with this population.
victoria: So I think of self-disclosure and countertransference being a, a, not a red flag. What's the word I'm trying to use? Something to consider just something that's coming into the room that we need to consider. For example, I'll get a lot of questions from therapists. I know you do too, [00:41:00] about, chronically ill.
How much do I self disclose to this client? And I think if you can justify either decision, that's great. I think you, something to consider is of course always the question, what is the purpose of why I'm sharing this? Is it more for my own understanding? Will this actually be helpful to the client? Um, so for example, some. Therapists, uh, I'll give the example of like EDS. So for, for therapists like myself, um, any type of hypermobility, it can present really, really differently in a lot of different bodies. Um, from really mild to really severe. And so my hypermobility might not be related to another person's hypermobility, right?
Like my advice might not be appropriate to another person just because we share the same diagnosis. So I think that's something therapists really need to be aware of, as well as like the ethical mandate of staying within our scope, both for social workers and counselors. What's always [00:42:00] important that we practice within our scope. Um, I'll also say, and, and maybe this is something you've seen too, is the field really changing around self-disclosure? You know, in, in grad school, we're always taught don't tell the clients any. In grad school, um, I, I once told like a, a. A fake client that we were practicing with. Um, oh, I, I remember what it was like to be a student and I got feedback that don't self disclose to a client.
So I think, um, at one point it was really, really strict that we don't self disclose to clients. And I see that kind of changing in the field where, what does it look like to self-disclose appropriately and, and helpfully, uh, for that client, um, especially if we're doing larger advocacy work, uh, whether in our practices or beyond. then I think, um, yeah. I'm curious, how do, how do you approach self-disclosure with your
Destiny Davis LPC CRC: Yeah, I mean, yeah. So, um, I definitely [00:43:00] actually start as early as my website and, um, I know that again, yeah, it's, that's a little bit controversial in the field. And, um, you know, the, the idea of not disclosing anything at all, uh, and being a blank slate only really works when you're a white male. And so that's really where that comes from, kind of early on in, in the field and.
As soon as you're any other identity people can start to, I mean, of course they can have assumptions about, about white men, but if you think back to that psychoanalytic Freud, Roger, I mean, Rogers wasn't psychoanalytic, but the, the founding fathers of psychology all white and male, and you can hide a lot about you and your personal inner workings as a white male.
It's a lot harder to do that as start, as soon as you start to have other intersections, whether that's the color of your skin or how you, you know, how you decide to dress or if you're female or, you know, there are ways to, um, I think there's a lot of nuance in this conversation, but my point is that it's, we already disclose just by being [00:44:00] female.
Sometimes we're disclosing certain things. Um, we already disclosed by, uh, um, yeah, again, the color of our skin can, can disclose certain things. So that in and of itself, I think is important to know why we have that role in the first place. And then in order to kind of then discern when do I disclose more details.
About me and my life, um, and why am I doing it? So I do disclose early on in my website. Not everybody reads the website. And so, um, you know, they may not, it's not like plastered from like head to toe on my website. So it's not like, you know, there's definitely clients who miss it. Um, but because we live with such dynamic conditions, as soon as I do let a client know, Hey, this is something I've struggled with as well, I get where you're coming from.
Um, after they've kind of explained something to me, this is never from the jump. Like, I'm not trying to rush in and make them feel seen and heard. And I mean, I'm not trying to rush in and make them feel like I have had the exact same experience as them. [00:45:00] What I am trying to do is saying, especially when they are really, really overexplaining a particular medical experience or a particular symptom, and I can tell that they are scared.
I don't understand. That is where I find it tends to be a lot more help to be like. I actually do live with chronic fatigue and migraine as well. Um, I usually will say a symptom over a diagnosis and as soon as I say that, if they kind of stop over explaining and they can actually just like actually finish the point of what they really wanted to say, that's when I know that was a helpful self-disclosure.
If they keep over explaining, then it might just be that they simply like want to be heard and they wanna explain things in their way and they wanna like get that, that point out the way they were saying it and it wasn't really about me, maybe not understanding, in which case I now regroup and like get that straight in my mind.
So, you know, as therapists we're always, I mean, I don't know about how about for you, but for me I'm always kind of like trying [00:46:00] to figure out what the client is saying and why and then reflecting that back to them and helping them gain a deeper understanding of themselves. So that's where, that was a long-winded answer of saying I do use self-disclosure and I'm very intentional about it.
victoria: the emotional labor there. Um, and you know, as you're talking, what it makes me think about is not heard a lot of examples of, um, what is it? I hear a lot of appropriate self-disclosure and it's hard to identify when something is going to land or not land until after it happens. Um, so for example, an example of inappropriate disclosure would you, would, might be you centering your medical experience and maybe coloring that client's. Own decisions. So for example, I'll have a lot of clients, um, and, and this has happened for, for me or for people that I've [00:47:00] mentored where they'll say, oh, I, I have the same disorder too.
And then the client will wanna know, well, what did you do for treatment? Who did you go to for treatment? and every single time I have, have given a suggestion very bluntly of like, I did this, it worked, or I didn't do this, it didn't work. Um, it, it has never worked. I, I just don't use that, that kind of self-disclosure anymore.
And the reason for that is I'm not a medical expert and I don't wanna color this client's decision making process. And it's so personal to that client, the medical decisions that we make, um, that I couldn't possibly give them an answer. Um, and, and that might, um. might be an example of when it would be inappropriate to disclose or maybe you have a client with, with OCD around medical decisions or that me, what is it that illness, OCD, medical anxiety where they are looking to you for kind of that validation or that feedback like compulsively of, have I made the right medical decision?
Have I made the right medical decision? And by you reinforcing that, it just might [00:48:00] not be appropriate for, for that kind of treatment. yeah. And then I think secondly, when we think about ethics, I think about counter transference. Ugh, gosh. is so difficult in this field, right? When we're working with clients, um, who are chronically ill or even terminally ill. Where it's so hard not to either see ourselves or family members, whether it's like a certain symptom or a certain diagnosis, just watching these clients, um, go through these medical systems and, and hear how maybe they're, they're struggling or, again, facing these barriers to wellness. Um, so I think one way to address that is, first of all, finding an excellent consultation group or maybe an excellent support group or support person for yourself. Um, destiny, I know you run an excellent free clinical consultation group for therapists who specialize in chronic illness, and I think that can be invaluable as a [00:49:00] space for you to process these very, very difficult cases that you're coming across. Um, if you're a therapist that specializes
Destiny Davis LPC CRC: Yeah. Yeah. And it could be difficult because of the, your own condition and, and you're trying to figure out the, the transference, countertransference of it all. Or it could be difficult just because there's so much grief and anxiety and trauma, uh, that that often go hand in hand. With having these conditions.
Um, yeah, so the self-disclosure, I all, you know, again, going back to exactly what you said, like it's not about centering yourself, but I use it as data to help me understand their inner world better. So I might, you know, slip a little like self-disclosure in there and then I'm watching for how they respond to that and listening for how that landed for them.
Um, and that just continues to gimme more data to work with in helping them reach the goals that they and I have, have set together.
victoria: therapists, I think about burnout and your [00:50:00] own wellness. use the word earlier, sustainable. talk about these wellness initiatives that I'll, I'll go over in more detail in this talk in Atlanta. Um, know, wellness is, is, is nothing for your clients if you can't maintain a, a semblance of your own wellness. And again, I know that's a really hard conversation for therapists because maybe that involves with you working less. It involves with you adding breaks into your schedule. And not everybody, every therapist has that option. Um, but when you are working with these really complex medical cases, um, it is so important that you take care of your brain and your body because that's it.
That is all that you have to do this work, um, is your brain and, and your body. So I always say it's so important for us to take care of ourselves cognitively. Because again, that is all that we have to do this work. And also, you're a person deserving of wellness. You don't just have to access [00:51:00] wellness to prevent burnout so that you can show up better and, and more and faster for clients.
It is also because you are a human deserving of wellness. Even if people don't see that around you. Um, it is so important that you
Destiny Davis LPC CRC: I completely agree. We really do have this like, you'll, you'll rest when you die or you will, you know, deserve you, you'll rest when you have deserved it. And it's, it's keeping us sick and burnt out.
victoria: works where we have to rest before we earn. I just kind of take the question, earn out of there when I'm talking about wellness for therapists, um, for clients. Um, because you, you have to rest. 'cause otherwise you can't do the work. Like, it's just mathematically doesn't work out that way.
Destiny Davis LPC CRC: Exactly. Is there anything else about like how therapists should [00:52:00] maybe approach conversations around accommodations with clients that comes to mind?
victoria: When I think about some of the trickier conversations that I've had around accommodations, clients feeling really disempowered by family or by workplaces. Um, by groups of friends, by their, their social and. I think it's so important when we're talking about accommodations and maybe barriers to them accessing accommodations, like, yes, we need to look at those systemic barriers. also interested in looking at self-esteem when you are in a body that needs a lot of compassion, you might have received a lot of messages that you're, you are somehow less than that. You are somehow, like you said earlier, less deserving. And I think if you are not taking care, like genuinely [00:53:00] caring for this, for your own self-esteem and, and self-worth, it can be really hard for you to even remember to use your accommodations. I'll give an example. Um, for any theme park enthusiasts that you have, um, as listeners, um. It was kind of the first time this summer where I was in a store at a theme park and I remember feeling just really overstimulated and having to sit down even just admitting to myself, oh, I'm really not doing okay, like I'm really weak right now. was kind of the first time that I had done that in my life where I was like, I actually don't have to force myself to do this. This isn't fun for me anymore. Even when I'm telling myself that this is fun, gonna take myself outside and spend too much money on a smoothie and sit down. and I know that that can be so, like, that's such a small [00:54:00] step, right? But when you are first looking at accommodations for yourself at prioritizing your wellness, even just admitting that there is a problem, right? Complaining first, um, might be the first step in you even remembering that accommodations are even an option for
Destiny Davis LPC CRC: Yeah, I met with a new colleague, a new, um, PT in town. It was such a wonderful meeting. She and I had a lot in common. Um, and you know, I've, I've really improved so many of my symptoms around chronic fatigue. Like, I, I used to not be able to like, finish a shower. Like, I, I couldn't wash my hair. I couldn't, I, I, you know, I wasn't going out anywhere.
Like the lockdown was a blessing for me to not have to drive anywhere and not go anywhere. And of course, um, not all blessings and not saying it was a positive experience, but like. When the world started to accommodate me because everybody was doing that, there was something there that I, I have to admit, was really nice.
I've come a long way probably [00:55:00] because I accommodate myself so much that I have more stamina now. Um, and the, the lady that I was meeting with, um, I, I could actually tell that she was getting really dysregulated, uh, but we were having a great conversation and so I knew it wasn't like that. It was probably the environment we were in, right.
And I can remember how many meetings I've had with friends and networking, et cetera, where I just stuck through. And then I would get to my car and collapse, like cry or, um, like just totally collapse and just sit there before I could even drive because I was so, I had gone way past my max and we were probably about 45 minutes into our conversation and, and she was like.
She was starting to wrap up the conversation like, okay, we're gonna, you know, like go or whatever. And then she's like, actually, can we just step out? Like, can we step out of the coffee shop? It's, I'm really overstimulated. And I was, and then we ended up talking for another, like 45 minutes outside of the coffee shop and I could just see the difference on her.[00:56:00]
Um, she was so much able, like less dysregulated. It was really, really beautiful to see somebody ask for what they need like that. Um, and to be on the other side of that where it's like, man, yeah. How many times could I have just asked friends, colleagues, et cetera, to just like, can we just step outside maybe instead of sitting here and this loud music, barely able to hear each other talk.
of us are probably overstimulated,
victoria: Yeah,
Destiny Davis LPC CRC: so.
victoria: of um,
yourself. Permission for that, or even just question that as an option. And I think, oh, this is what you said. Who does? Who does she think she is? And I think if we're having that emotional reaction to somebody bluntly saying, I'm gonna do this for my body or my brain, and if we're having the reaction of who do we think she is, that says more maybe about our own needs not getting met than it does about the other
Destiny Davis LPC CRC: Obviously you and I feel very strongly about just being, feeling well, being able to feel [00:57:00] well, even if you're not, you know, quote unquote healthy. You still have your condition, you're not cured, but we believe in being, bringing wellness wherever you can, um, and, and accommodating where you can.
So maybe this is a great time to talk about the accommodations that we're offering at our conference in an effort to, no one has to ask for this. These are just built in.
victoria: you guys can find me in the sensory room in between sessions. We are so excited to have a full destiny. I know you, uh, toured the, the physical space. Um, we are so excited to have a, a fully separate, I believe, sensory friendly room, um, where we'll have low lighting, we'll have places for you to sit and stretch out. Um, and just a really nice space where you can feel like you don't have to perform a certain way with your body, right? So I'm really excited for that sensory friendly space and also for our neurodivergent people as well. We know there's a big crossover between chronic health issues and neurodivergence. [00:58:00] Um, so first and foremost, I'm just really excited for this sensory room. Um, we'll also be having accommodations such as like large print, large type, um, captions on, on all of our speakers, um, for all of our speakers as well. Um, I also think just having a virtual option in and of itself can be a huge accommodation.
I, I love the ability that you get that choice. If you wanna go in person with accommodations, that's fantastic. If you need accommodations from your home, you need to do it from your bed. That is also an accommodation. So just having that choice and that option can be huge. Um, any other accommodations that you can think
Destiny Davis LPC CRC: Yeah, we'll have a fragrance environment. Um, also we'll have an accessibility coordinator, so this will be one of our volunteers who has access to our, I haven't decided yet if it'll be like in a WhatsApp or something like that. But it will be a dedicated text line so that yes, you, there will be volunteers around who can answer your questions, but you can also just text it [00:59:00] quickly so that it's accessible.
Um, and you don't have to like search for where the volunteers are. we'll also have a lot of flexible seating arrangements. So the room that we have is double the size of the maximum number of participants that we will have. So there's a lot going to be a lot of room for like, you can sit on the floor. I plan on actually having a ton of blankets and pillows there so that you can, like we were talking about earlier, just be flexible.
You don't have to be sitting in this hard seat for like, you know, ever, um, hurting your back like my, like mine. So, um, lots of breaks built into between each and every talk. There's a 15 minute break. I know a lot of times conferences try to go back to back, to back to back because they're trying to get the most in, but we will still have 13 hours over two days with 15 minute breaks in between each talk.
Um, I do think there's one one hour talk that goes back to back, but, so don't quote me, but for the most part we have 15 minute in between each. Um. [01:00:00] As well as of course, like the ADA compliance stuff like, you know, there's elevators and, and things like that. It is on a second floor, but there will be elevators.
we'll also have, um, KN N95 masks and everyone's welcome bag that they are welcome to use as well as air purifiers throughout the space. and then. Lastly, something that's really exciting. Um, we were just kind of having fun with it, but we've al already had people purchase this package and it's called the Executive Function Functioning Package or EFP.
Um, and so this is where you will get two conference tickets. So one for you and one for your favorite colleague or person of your choice. Um, but they will also be able to attend the conference, get CEEs, things like that. So we kind of designed it thinking you might bring a colleague along. Again, that could be another therapist or a physical therapist.
We have CEEs available for them as well. As well as in this package, we will buy your ho your hotel room, three nights with two full beds and in the room. So one hotel room, gluten-free and nut [01:01:00] free. We forgot to mention that, but the entire conference will be gluten-free and nut free, um, that's fine.
That actually gives us a little bit.
victoria: told me about the executive functioning package, I was like, why is that Not at every, every event I've ever gone to because I would 1000% purchase this for myself or every conference I go to. again, it's all transportation taken care of to and from the airport. Um, your hotel room is booked. You're gonna have, uh, just that personal high touch experience even for touring stuff. Um, outside of the conference, I think Destiny, you're in Atlanta. You can speak a little bit more to that, but we'll also have the Atlanta, is it the Atlanta Fun Pass?
Destiny Davis LPC CRC: Yeah, there's also an Atlanta City Pass, and so this is valid from nine days of first use. So you could stay, you could come before the conference, day after, and you have nine days to use this pass. We're giving you two of those in the EFP package. The EF package. [01:02:00] Um, you'll get access to the Georgia Aquarium, the Atlanta Zoo World of Coca-Cola, Fern Bank, museum of Natural History, Georgia Football Hall of Fame, and the National Center for Civil and Human Rights.
So it's basically all of our biggest Atlanta attractions, and you will get a free pass to all of those for two people. So this is a really cool, and yeah, exactly like you said, like we will, if, if you're not renting a car, if you're not driving in, we will pick you up. From the airport. Um, we will, we will arrange transportation to and from the airport for you and, um, as well as one night of comp to dinner.
So lots of stuff involved in this package and, and one of our amazing assistants or volunteers is gonna help coordinate a lot of that and you'll be able to, like I said, with that dedicated text line, you'll be able to ask questions there. Like, we just really want people to come and feel one welcome in Atlanta.
I love my city and, um, there's so much to offer here in terms of hospitality. Um, and so I wanna [01:03:00] extend that to all of our guests who are coming from out of state.
victoria: we wanted to do this conference. We really wanted it to be a, a national experience that therapists from all over the US could attend. what I do love about Atlanta is just the accessibility. You know, we were very careful about where we chose. Especially with, uh, the airport in Atlanta.
And look, I've gone through the Atlanta airport. Um, it, it can be a lot. There's so many accommodations already built in, um, and a hub for like ev everywhere in, in the, so across the us. And so something again that the reason that we chose this city that we chose this hotel, um, was due to the accommodations.
And we could just not be more excited to see everybody in person. Uh, March 6th through seventh in Atlanta, Georgia.
Destiny Davis LPC CRC: Yes. I'm so excited. So that concludes today's episode. Um, I cannot wait to, yeah, one publish this episode. People can really get a taste of what our [01:04:00] conference is gonna bring. And, um, yeah, I'll put all of your information in the show notes and people can sign up for your, for your workshops as well, whether it's upcoming or past.
So,
yes,
victoria: much, destiny.
Thanks for listening. If you learned something new today, consider writing it down in your phone notes or journal and make that new neural pathway light up. Better yet, I'd love to hear from you. Send me a DM on Instagram, email me or leave a voice memo for us to play on the next show. The way you summarize your takeaways can be the perfect little soundbite that someone else might need.
And lastly, leaving a review really helps others find this podcast, so please do if you found this episode helpful. NPS Clicking, subscribe ensures you'll be here for the next episode. See you [01:05:00] then.
Dr. Victoria Rodriguez (she/her/hers) is a Licensed Professional Counselor in New Orleans, Louisiana, and recipient of the 2024 Louisiana Counseling Association Distinguished Professional Service Award. Named the 2023 Outstanding Doctoral Student by the Gamma chapter of Chi Sigma Iota, Victoria specializes in medical trauma in her private practice and provides trainings on wellness for professionals and healthcare organizations. She serves on the Pregnancy Associated Mortality Review Board with the Louisiana Department of Health to improve equitable medical care in Louisiana. At the Chronic Illness Therapist Conference, Victoria will explore the systemic, institutional, and interpersonal barriers that impact wellness for chronically ill and disabled clients, examining how supporting client wellness influences therapeutic outcomes and career sustainability while navigating the ethical considerations unique to this work.
Meet Destiny - The host of The Chronic Illness Therapist Podcast and a licensed mental health therapist in the states of Georgia and Florida. Destiny offers traditional 50-minute therapy sessions as well as therapy intensives and monthly online workshops for the chronic illness community.
Destiny Davis, LPC CRC, is solely responsible for the content of this article. The views expressed herein may or may not necessarily reflect the opinions of Dr. Laurie Dos Santos.